News
Novel Precision Medicine Trial for Metastatic Pancreatic Cancer
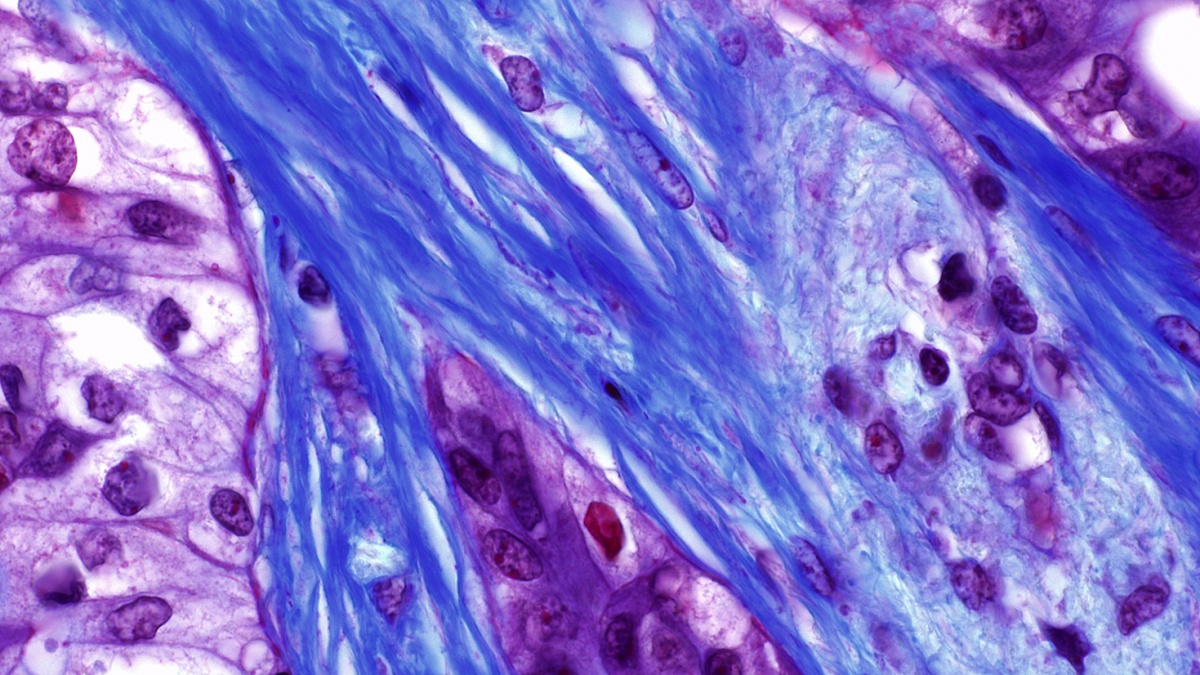
Shown here, a human pancreatic tumor stained with Masson's trichrome; Image credit: Dr. Kenneth Olive
The Lustgarten Foundation has awarded Columbia University’s Herbert Irving Comprehensive Cancer Center (HICCC) a three-year grant, as part of its Translational Clinical Program, to test a new precision medicine approach to the treatment of metastatic pancreatic cancer.
“The prevailing model in personalized cancer treatment is to attack the DNA mutations that are believed to be driving an individual patient’s tumor,” says principal investigator Kenneth P. Olive, PhD , assistant professor of medicine and pathology & cell biology at HICCC. “While this approach has been astonishingly effective for a handful of rare cancers, we expect it will only work for a very small fraction of patients with the most common types of cancer.”
Pancreatic ductal carcinoma (PDA)—the most common form of pancreatic cancer—is a case in point. Researchers have identified few genetic drivers in pancreatic tumors, and the most common driver ( KRAS ) is not easily targeted. Conservatively, only about 15 percent of PDA patients are likely to benefit from conventional DNA mutation-based precision medicine therapies and most of these will either not respond or will relapse with a drug-resistant form of the disease.
“Our study takes an entirely new approach,” says Dr. Olive. “Instead of looking at the mutations encoded in a tumor’s DNA, we analyze the tumor’s RNA. Since RNA is the tissue-specific ‘working copy’ of a cancer cell’s DNA, it’s a more accurate reflection of the genetic programs that are active in a tumor and critical for its survival. We can then match the patient to approved and investigational drugs that inhibit those programs.”
The approach for matching patients to drugs based on their tumor RNA was developed by Andrea Califano, Dr. , chair of the Department of Systems Biology and a co-leader of the grant. In preliminary tests of this approach—called OncoTreat—on PDA tumor samples, the researchers identified at least one matching drug for 85 percent of patients. The approach has also been tested on other cancers and is the first NYS Department of Health CLIA approved RNA-based test to match patients to the full repertoire of FDA-approved and investigational drugs in phase 2 and phase 3 clinical trials. To date, three of four patients who received OncoTreat therapy have exhibited clinical responses.
“OncoTreat identifies drugs that can invert the activity of a novel class of cryptic cancer targets, called master regulator proteins,” says Dr. Califano. “These proteins, which are conserved within large subsets of cancer patients and represent the ‘engine room’ of the cancer cell, are responsible for integrating the effect of individual genomic alterations and for making the cancer cell impervious to a wide range of perturbations, including those resulting from conventional drug treatment. By targeting the ‘engine room’ of the cancer cell, we hope to develop more universal and more effective treatment.”
The primary goal of this phase 1b clinical trial is to assess anti-cancer activity of OncoTreat-predicted drugs in 30 patients with recurrent PDA, on an individual patient basis. The grant will also support preclinical studies to develop optimized two-drug regimens for groups of PDA patients based on their OncoTreat profile. The program comprises a multidisciplinary team of clinicians, experimental biologists, and computational biologists working in close collaboration to deploy an entirely new approach to precision medicine in pancreatic cancer.
“PDA is a highly lethal disease with no truly effective treatment options,” says Dr. Olive. “New approaches to this disease are desperately needed.”
The Lustgarten Foundation, based in Woodbury, NY, is a leading private foundation dedicated to funding pancreatic cancer research.